The role of data mapping in interoperability in healthcare
All of us like that feeling when some stuff matches another one, whether it is a match between you and your soulmate, your shoes and belt, or white wine and cheese fondue. Likewise, in the healthcare industry, there is a match between interoperability and data mapping, where the latter helps ensure a smooth flow of information among different healthcare systems, e.g., Electronic Health Record (EHR)/Electronic Medical Record (EMR) systems, and technologies to connect, share, and make use of health information.
Some interesting figures: According to Statista, in 2021, 91 percent of hospitals in the United States reported they sent care record summaries electronically to systems outside of their organization, marking a slight increase from 2017. The share of hospitals in the U.S. that engaged in all four domains of interoperability increased from 41 percent in 2017 to 62 percent in 2021. Plus, about 90 percent of hospitals and physicians use EHR systems.

In the complex web of medical information, data mapping emerges as a critical player. It serves as the bridge, connecting disparate healthcare systems, telemedicine or other, and laying the foundation for a more integrated and patient-centric approach to healthcare delivery. In the following sections, we will discuss how data mapping serves as the linchpin of interoperability, deciphering the complexity of healthcare data and enabling a seamless exchange of information for the benefit of patients and healthcare providers alike.
What is interoperability in healthcare?
A few more words about the meaning of interoperability in healthcare. Interoperability in healthcare is the ability of different information technology systems and software applications to communicate, exchange, and use data in a coordinated manner. Achieving interoperability is essential for enhancing personalized patient care, reducing medical errors, and improving overall healthcare efficiency.
In a highly complex healthcare ecosystem, where information is generated and processed across various platforms and devices, interoperability serves as the root, allowing for efficient communication and coordination among various stakeholders, including healthcare providers, payers, and patients.
What are the benefits of interoperability in healthcare?
Interoperability in healthcare is not just a technological advancement; it is a transformative force that improves patient care, enhances efficiency, and promotes collaboration across the entire healthcare landscape. The benefits extend beyond individual patient encounters to impact public health, research, and the overall effectiveness of the healthcare system. Let’s look at some of them:
- Enhanced care coordination: as stated above, the main benefit of interoperability is enhanced coordination. It ensures the exchange of patient information among different healthcare systems. This way, healthcare providers have access to comprehensive and up-to-date data, leading to more coordinated and effective care.
- Reduced medical errors: access to complete patient records and medical histories enables healthcare professionals to make well-informed decisions. This, in turn, reduces the likelihood of medical errors, as providers can avoid duplicate tests, conflicting medications, and other potential pitfalls.
- Improved patient outcomes: interoperability supports a holistic view of a patient’s health history, enabling personalized and targeted treatments. This personalized approach contributes to better patient outcomes and overall satisfaction.
- Streamlined workflows: efficient data exchange among different healthcare systems reduces administrative burden and streamlines workflows. Healthcare providers can spend more time focusing on patient care rather than navigating through disparate systems and manually managing data.
- Cost savings: by avoiding redundant tests and improving overall efficiency, interoperability can lead to cost savings for healthcare organizations and patients. It contributes to a more cost-effective healthcare delivery system.
- Research and innovation: Interoperable systems facilitate access to large datasets, fostering medical research and innovation. Researchers can analyze aggregated data to identify trends, conduct clinical trials, and make advancements in medical knowledge.
What is data mapping in healthcare?
And a little bit more attention to data mapping. Data mapping is a critical process that involves establishing a connection between data elements in one system to their corresponding elements in another system. It serves as a linguistic bridge, enabling the accurate translation and interpretation of health-related information as it moves across various healthcare systems, such as EHRs, laboratory information systems, and other medical databases.
Get the best of data mapping to contribute a lot to healthcare interoperability
How to improve interoperability in healthcare with data mapping?
In the context of healthcare interoperability, data mapping emerges as a versatile tool capable of addressing challenges at various levels. By tailoring mapping solutions to foundational, structural, semantic, and organizational layers, healthcare stakeholders can pave the way for a more connected and patient-centric healthcare environment. Let’s see how it works in practice.
Data mapping steps for healthcare interoperability challenges
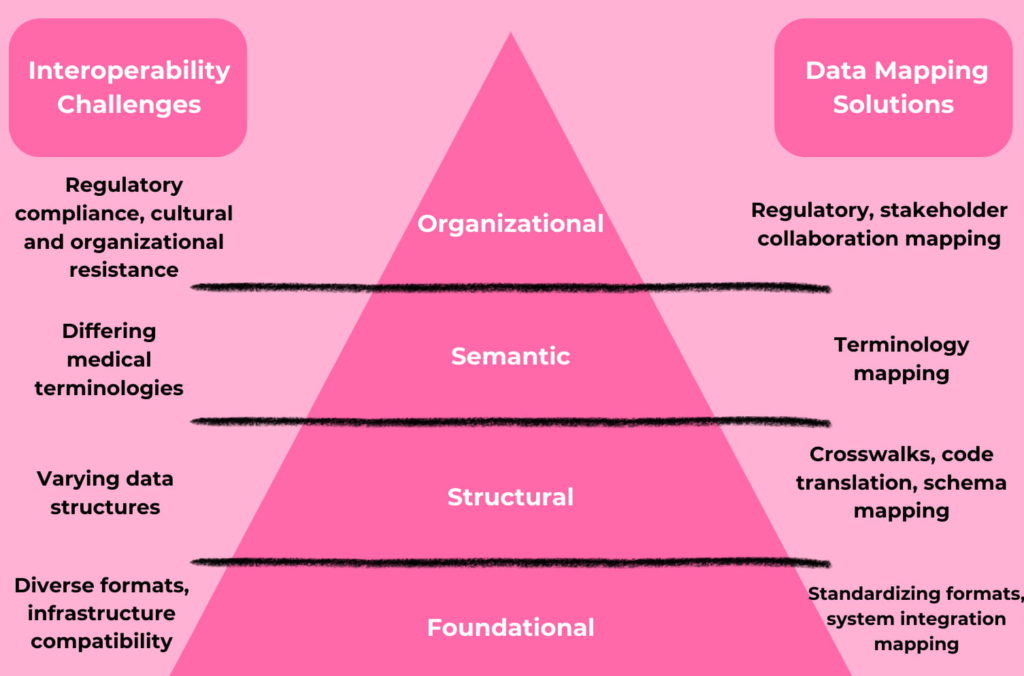
Foundational level:
- Interoperability challenge No. 1: At the foundational level, the challenge lies in establishing a basic level of connectivity and data-sharing capabilities. Healthcare systems often use different technologies and protocols, hindering the seamless exchange of information.
- Data mapping solution: Implementing a standardized data format, such as Fast Healthcare Interoperability Resources (FHIR), facilitates basic data exchange. Data mapping ensures that the data structures in different systems are aligned to this standard, allowing for foundational interoperability.
- Interoperability challenge No. 2: Infrastructure compatibility, i.e. variability in the underlying infrastructure of healthcare systems can impede interoperability efforts.
- Data mapping solution: System integration mapping, which stands for mapping data elements that facilitate cross-system integration and utilizing middleware solutions to bridge the gap between disparate infrastructures.
Structural level:
- Interoperability challenge: Structural interoperability involves the organization of data and the way it is formatted. Variability in data structures, coding systems, and terminologies can impede effective communication between different healthcare systems.
- Data mapping solution: Creating crosswalks between different coding systems and terminologies, ensuring that data elements are accurately translated from one structure to another. This helps maintain structural integrity during data exchange.
- Data mapping solution: Adopting canonical data models establishes a common representation of healthcare data. Data mapping aligns disparate structural models to this canonical format, promoting consistent data organization across systems.
- Data mapping solution: Schema mapping, which stands for employing schema mapping to align the structure of data elements between systems and creating mappings that define relationships between different data structures.
Semantic level:
- Interoperability challenge: Healthcare entities may use different coding systems and medical terminologies, leading to potential misinterpretation. Differences in the interpretation of medical terms and concepts pose a significant challenge at this level.
- Data mapping solution: Data mapping enables the creation of mappings between different terminologies and coding systems. This ensures that the semantic meaning of medical information is preserved, allowing for accurate interpretation by diverse healthcare systems.
- Data mapping solution: Implementing a shared ontology—a structured framework for representing knowledge—facilitates semantic interoperability. Data mapping aligns disparate ontologies, ensuring a common understanding of healthcare concepts.
Organizational level:
- Interoperability challenge No. 1: Regulatory compliance, i.e. adhering to diverse and evolving regulatory standards poses challenges for interoperability.
- Data mapping solution: Regulatory mapping, which stands for creating mappings that align data exchange processes with regulatory requirements and implementing data governance frameworks to ensure compliance.
- Interoperability challenge No. 2: Organizational interoperability involves addressing cultural, legal, and policy barriers that may hinder data sharing among healthcare organizations. Privacy concerns, varying data governance practices, and regulatory differences are common challenges at this level.
- Data mapping solution: Stakeholder collaboration mapping, which refers to facilitating collaboration through data mapping to address organizational resistance and establishing clear communication channels and incentives for data sharing.
- Data mapping solution: Data mapping can assist in aligning data-sharing policies and practices among organizations. This ensures that data exchange adheres to regulatory requirements and organizational policies, promoting a harmonized approach to interoperability.
Data mapping for EHR interoperability
Summing up data mapping solutions, let’s finish with the most practical thing, namely: its contribution to EHR interoperability. The most crucial aspect of data mapping for EHR and EMR interoperability lies in its ability to establish a standardized and coherent language for the exchange of patient information across diverse healthcare systems. It aligns data between the source and target systems. Moreover, the mapped data is also used for data integration, cleansing, migration, and ETL purposes.
Data mapping tools
And the last important thing shall be a data mapping tool selection. You can consider the following tools, however, it’s also essential to consider factors such as the specific data formats supported, ease of use, scalability, and integration capabilities with existing healthcare systems:
- Talend Open Studio: Talend offers an open-source data integration tool that includes powerful data mapping capabilities. It supports ETL (Extract, Transform, Load) processes and provides a user-friendly interface for designing and executing data mappings.
- IBM InfoSphere DataStage: IBM InfoSphere DataStage is an enterprise-level data integration tool that includes robust data mapping features. It allows users to design, run, and monitor complex data integration processes and supports various data sources and targets.
- Oracle Data Integrator (ODI): ODI is a comprehensive data integration tool provided by Oracle. It includes data mapping capabilities along with features for data extraction, transformation, and loading. ODI is well-suited for organizations using Oracle databases.
- Informatica PowerCenter: Informatica PowerCenter is a robust data integration and mapping tool widely recognized for its comprehensive features, user-friendly interface, and capabilities for data transformation, connectivity to various data sources, and metadata management. It supports various data formats, including XML, databases, flat files, and more.
Conclusion: data mapping best practices equal healthcare interoperability solutions
So, the standardization of data formats, schema mapping for structural alignment, terminology mapping for semantic consistency, and identity mapping for consistent identification, collectively contribute to the establishment of a common language and a shared understanding of healthcare data. This standardization not only enables cross-system integration, allowing healthcare professionals to access comprehensive patient data seamlessly but also ensures compliance with regulatory requirements, fostering a culture of data governance and accountability.
In essence, the systematic application of data mapping principles emerges as a foundational element in navigating the complexities of healthcare data, contributing to a more interconnected, patient-centric, and compliant healthcare ecosystem.