How effective is a patient management system in chronic care?
In the modern world, the most common causes of death vary from heart disease, cancer, chronic lung disease, stroke, Alzheimer’s disease, and diabetes, to chronic kidney disease. The healthcare industry is overloaded with an influx of patients, particularly those requiring long-term care for chronic conditions. The breadth of potential health challenges has not only multiplied but has also intensified, turning the spotlight on the critical issue of chronic conditions that pervade societies globally.
Some interesting figures: 6 in 10 adults in the US have a chronic disease. Chronic diseases are the leading causes of death in the US. It is also responsible for nearly 90% of the nation’s $4.1 trillion in annual healthcare expenditures, according to the Centers for Disease Control and Prevention.
Unfortunately, this is huge. As the healthcare industry grapples with this overwhelming scenario, a crucial question emerges: how can this colossal burden be mitigated? The answer lies, at least in part, in preventive and management measures. It is within this context that patient management systems come into focus. In this article, we unveil the potential of patient management systems as innovative tools that could revolutionize the way chronic diseases are approached, managed, and, ultimately, mitigated.
Shape chronic care by unleashing the power of patient management systems
Issues in chronic care management
The management of chronic conditions requires continuous monitoring, timely interventions, and collaborative efforts between healthcare professionals and patients. As technology continues to advance, artificial intelligence, machine learning, Internet of Things, telemedicine and telehealth solutions are likely to further enhance the effectiveness of chronic care management. But that is not enough.
Traditional healthcare models often struggle to provide seamless and personalized care for individuals with chronic illnesses, necessitating the need for innovative solutions like patient management systems.
Reasons why you need chronic care management software
Enhanced care coordination platform
Care coordination systems facilitate improved communication and coordination among healthcare providers involved in a patient’s care. In a multidisciplinary approach to chronic care, various healthcare professionals, such as primary care physicians, specialists, nurses, and dietitians, are involved in a patient’s treatment.
Electronic Health Records (EHRs) allow seamless sharing of patient information, reducing the likelihood of medical errors and ensuring that all members of the healthcare team are on the same page regarding the patient’s condition and treatment plan.
Improved patient engagement platform
Patient engagement tools empower individuals to actively participate in their care. Through secure patient portals and mobile applications, patients can access their health records, receive educational materials, and communicate with their healthcare providers. This increased engagement fosters a sense of ownership over one’s health and encourages adherence to treatment plans.
Remote patient monitoring software
One of the key peculiarities of the patient management system is remote patient monitoring. This functionality enables healthcare providers to track patients’ vital signs, medication adherence, and other relevant health data in real time. Remote monitoring not only enhances the efficiency of care but also allows for early detection of potential issues, enabling timely interventions and preventing complications.
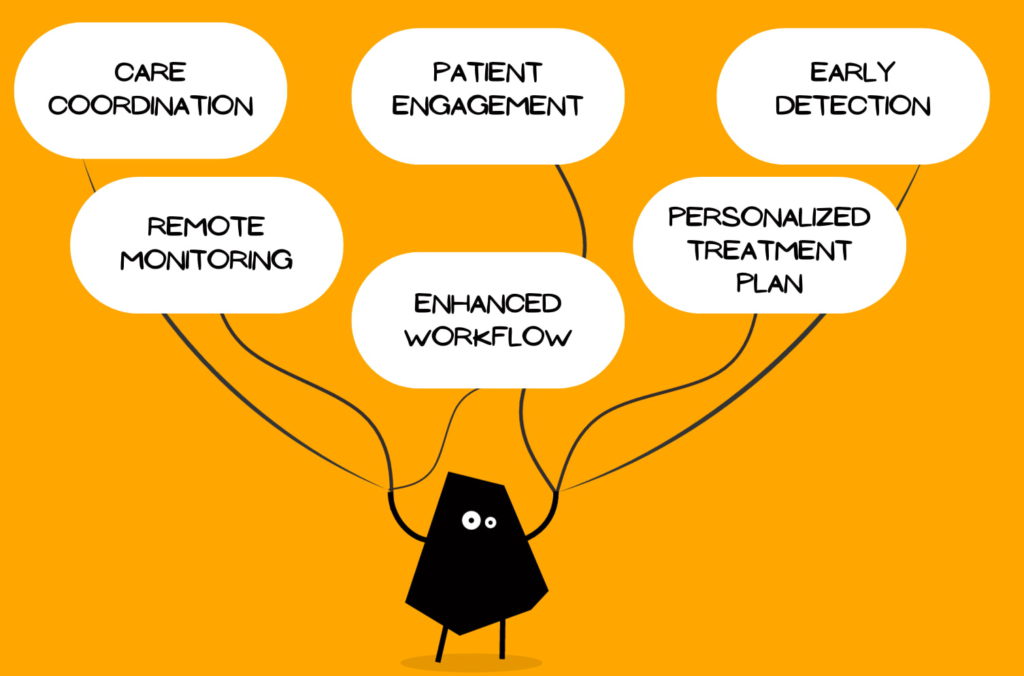
Benefits of using chronic disease management software
- Early detection and intervention: The real-time monitoring capabilities of the patient management system enable early detection of deviations from normal health parameters, allowing healthcare providers to identify potential issues before they escalate. Timely interventions based on data-driven insights can prevent complications, reducing the risk of hospitalizations and emergency situations. This proactive approach is particularly crucial in monitoring and managing chronic conditions effectively.
- Personalized treatment plans: Patient management systems leverage data analytics and artificial intelligence to analyze patient information and generate personalized treatment plans. Tailored interventions based on individual health data can significantly improve outcomes in chronic care. These systems take into account factors such as lifestyle, medication history, and patient preferences to create comprehensive and effective treatment strategies.
- Efficient workflow: By streamlining workflows and facilitating disease monitoring, chronic disease management software optimizes resource utilization. This efficiency is crucial in an overloaded healthcare system, allowing providers to allocate resources reasonably and improve overall patient care.
What features in the patient management system could be helpful?
By incorporating helpful features, the patient management system can effectively address the complexities of long-term care, promoting proactive, patient-centered, and data-driven approaches to improve outcomes for individuals with chronic conditions. Here are key features that could be instrumental in developing custom patient management software and beneficial for both healthcare providers and patients:
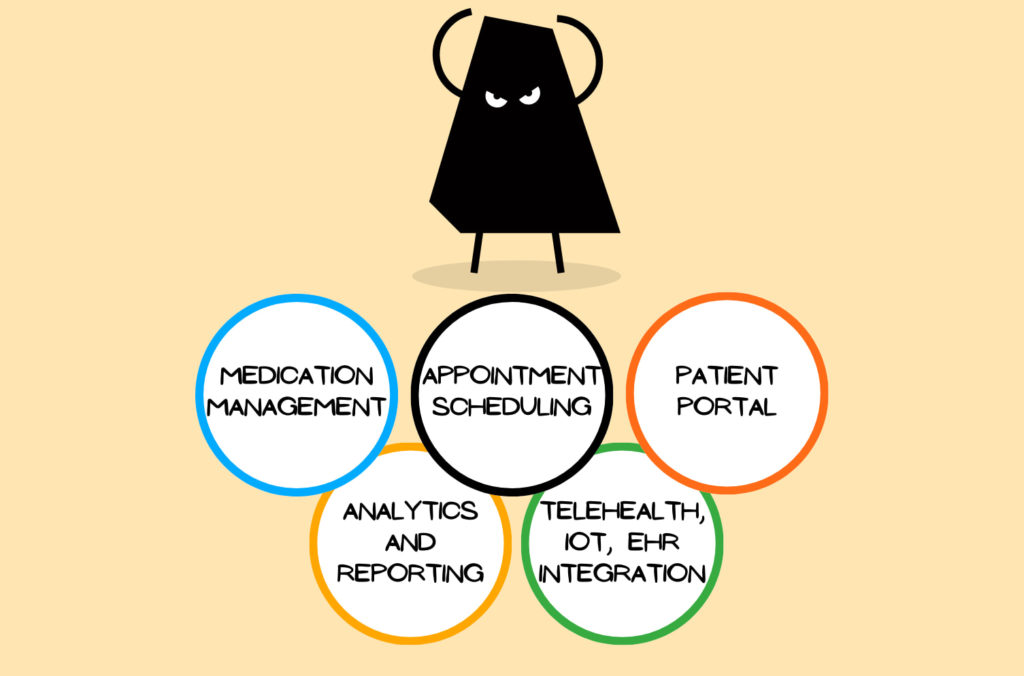
Appointment scheduling
- Integrated scheduler: allowing patients to schedule appointments, receive reminders, and access virtual waiting rooms for telehealth appointments.
- Appointment history: maintaining a record of past and upcoming appointments for reference.
Medication management
- Medication tracking: tracking of medication adherence and dosages.
- Medication reminders: customizable medication reminders to improve adherence.
Comprehensive condition monitoring
- Symptom tracking: patients can be able to log and track symptoms, providing healthcare providers with valuable insights via condition monitoring software.
- Disease-specific modules: specialized modules for diseases such as diabetes, cardiovascular conditions, and respiratory diseases.
Patient and healthcare professional portal
- Secure access: providing patients and healthcare professionals with a secure portal to access their health records, treatment plans, and educational materials.
- Communication tools: include messaging features for secure communication between patients and healthcare providers.
- Role-based access: assigning different access levels to ensure that relevant users have access to relevant information.
Disease monitoring
- Real-time data collection: continuous monitoring of vital signs, symptoms, disease flow, and relevant health metrics.
- Alerts and notifications: automated alerts for healthcare providers to intervene promptly based on deviations from predefined health parameters.
Telehealth and telemedicine integration
- Video consultations: support of secure video consultations between healthcare providers and patients.
- Document sharing: the sharing of documents, test results, and images during virtual appointments.
Electronic Health Records (EHR) integration
- Seamless data sharing: integration with existing EHR systems for streamlined access to comprehensive patient information.
- Interoperability: Support of interoperability standards to facilitate data exchange with various healthcare systems.
Integration with wearables and IoT devices
- Device connectivity: integration with wearables and Internet of Things (IoT) devices to capture real-time health data.
- Biometric data: collection and analysis of data from devices measuring parameters like heart rate, glucose levels, and physical activity.
Care plan customization
- Personalized treatment plans: healthcare providers can be allowed to create and customize treatment plans tailored to individual patient needs.
- Goal setting: features for setting and tracking health-related goals, promoting patient engagement.
Analytics and reporting
- Data analytics: utilizing data analytics to derive insights from patient data, aiding in evidence-based decision-making.
- Custom reports: generating customizable reports on patient outcomes, adherence, and overall health trends.
Scalability and flexibility
- Scalable architecture: capability to scale with the growth of patient data and increasing user numbers.
- Customization options: customization features to adapt the software to different healthcare settings and specialties.
Conclusion
To wrap things up, patient management systems have shown great promise in revolutionizing chronic care, offering a holistic and patient-centric approach. So, it’s quite effective. The adoption of patient management systems represents a significant step forward in improving the quality of care for individuals with chronic conditions. The potential benefits, including enhanced communication, personalized treatment plans, and improved patient engagement, make these systems a valuable asset in the ongoing efforts to manage chronic diseases effectively.
As healthcare continues to evolve, the integration of technology will play an increasingly pivotal role in shaping the future of chronic care management. If you are afraid that these technology advancements affect your compliance or data security, don’t worry, we’ve already examined what impact AI and IoT will have on healthcare data security. And spoiler – a forecast is comforting. Let’s make the difference together, reach out to us to discuss your ideas or questions. See you soon!