Filling in the Blanks in Population Health Management Systems. Why Data Analytics Is the Answer

Meet Dr. Jordan, a family physician. Dr. Jordan suspects that overexposure to dust in local pottery poses a life-threatening hazard to the staff and their families. When one of the facility workers is sent back home with a persistent, whooshing cough, the physician visits him in a congested tenement apartment where he lives with his wife and their little children. Dr. Jordan advises them to take simple precautions to prevent the spread of what he believes to be Mycobacterium Tuberculosis. Regrettably, as the family takes no heed of his warning, the disease soon takes a deadly toll on their youngest child.
This dismal story makes the plot of a 1914 tuberculosis awareness clip by The Edison Company. Since its creation, preventive care has reached another level with an array of advanced technologies that actively monitor and manage population health. Nevertheless, a significant number of healthcare providers still fail in deriving tangible value from Population Health Management systems. Confronted with massive volumes of unstructured data at hand, they find PHM solutions inadequate to solve the full range of their requirements.

The Temple Of Moloch (1914). Source: https://www.youtube.com/c/OldTVTime/
Population health management has come a long way since 1914, but without a robust, data-oriented strategy some of its challenges remain unresolved
How to Find Signals in the Noise? Challenges of Modern PHM Solutions
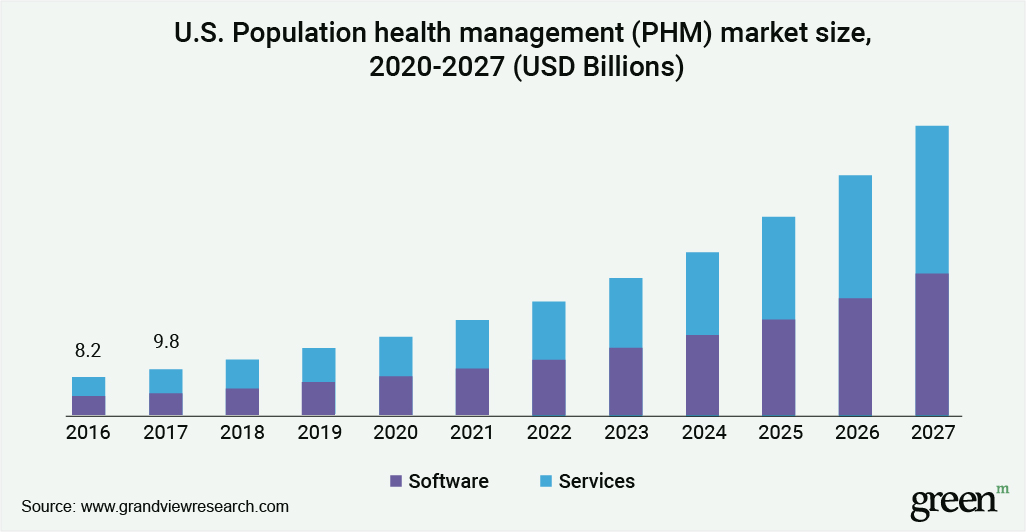
By 2027, the Population Health Management market is expected to surpass $150 billion. Companies and organizations dedicated to collecting, storing, scoring, protecting and targeting interventions based on population health data are gaining massive traction. However, access to detail-rich patient data alone is insufficient to close healthcare gaps effectively.
If PHM solutions are to support payers and providers with an accurate evaluation of community health trends, they must bridge population health data and advanced data analytics. Only this way will they advance from pure data aggregation and visualization to delivering actionable insights that unlock preventative healthcare. In particular, PHM platforms need to tackle the following issues:
Standardizing and structuring data
The first and foremost challenge for PHM is the steady growth of healthcare information technology, which leads to the proliferation of data sources. These include normalized clinical data, social determinants of health, lab results, pharmacy data, claims-based data, and more.
The volume of information generated in the medical industry expands so rapidly that by 2025 the estimated amount of healthcare data is projected to surpass this in the media and entertainment sector. What’s more, the specific groups of focus in population health management are continually evolving, imposing constant updates in the types of data used for analytics.
Using data effectively in care management decision-making means understanding what sources to pull data from, as well as how to organize the accumulated knowledge. Unfortunately, faced with such a breadth of information, healthcare providers often find themselves overwhelmed by the task. Additionally, the lack of common clinical vocabulary across disparate systems results in ambiguous data coding and categorization, fragmented Clinical Decision Support, and incorrect medication mapping.
Achieving near real-time data processing
The ability to keep track of community health data has a tangible effect on patient outcomes. For instance, one study by Health Affairs found that in two Ohio neighborhoods, the availability of real-time EHR data helped identify equity gaps in pediatrics and apply proactive health interventions, reducing hospitalization rates by 20%.
However, to support proactive, data-driven healthcare decision making, PHM solutions must be timely. At the minimum, they need to provide ad-hoc analysis of data across all geographies and cohorts, integrate clinical, financial and administrative information in near real-time, and supply on-demand reporting. Without these capabilities, healthcare professionals run into the risk of acting on outdated information, without even realizing it.
Biased risk stratification
Traditional Population Health Management systems tend to focus primarily on catering to high-risk patients, without accounting for communities with moderate and low health risks. This results from the limitations of clinical and claims data; clinical research usually spans only acute care; claims data, on the other hand, is highly retrospective and also captures a point in time rather than the entire care continuum.
Such fragmented — and biased — risk stratification leads to short-lived medical strategies that fail to address long-term health risks in communities. If we couple this with the fact that there are over 100,000 human services nonprofits in the USA (most of which aren’t regularly updating their community information), the threat of misalignment between provider care plans and population health requirements becomes more prominent. Even if a medical facility uses a cutting-edge PHM solution, it often isn’t capable of producing an exhaustive public health risk assessment because of the system’s inadequate predictive capabilities.
To proactively manage health for patients with lower risk scores, modern PHM systems need to leverage industry-recognized risk models, such as HCC, CDPS, Johns Hopkins ACG, etc. Used in conjunction with advanced data discovery techniques, they allow medical providers to develop more comprehensive prevention initiatives that include communities with existing and anticipated health risks.
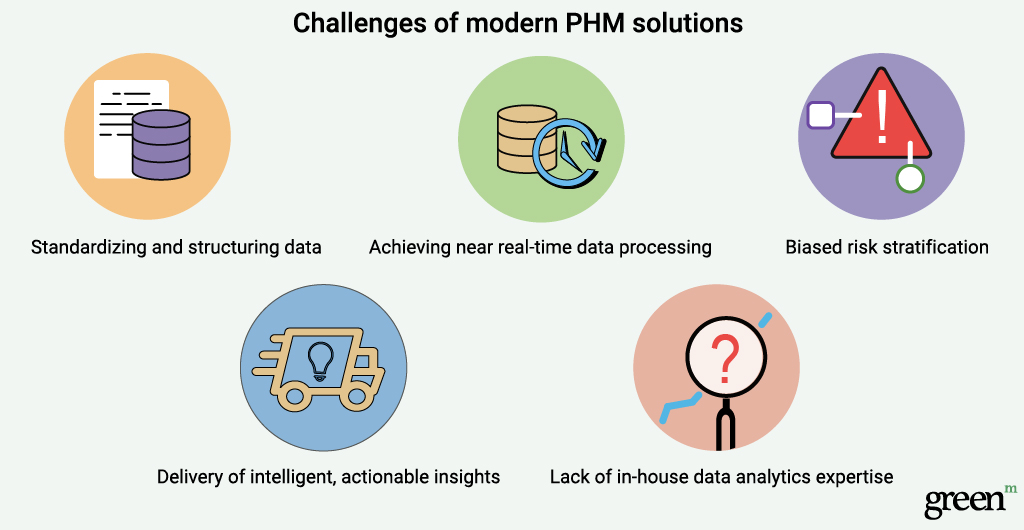
Delivery of intelligent, actionable insights
The ultimate goal of PHM is to offer a prescriptive approach to managing community health, where medical professionals are guided by analytical insights to monitor and act on care gaps and requirements proactively. In reality, though, most PHM systems work by validating already existing hypotheses of medical staff rather than contributing independent recommendations.
That’s where machine intelligence steps in. Instead of simply corroborating what doctors already know, AI-based PHM solutions apply sophisticated risk prediction models that actively look for hidden patterns in data to provide actionable forecasts. They help medical professionals flag and detect early-stage risks among unique sub-populations and target patients who would otherwise stay off the radar until the first symptoms develop.
One real-life example of the impact of AI services on patient outcome prediction comes from 2018 research, which explored the efficiency of AI-based EMR-based prediction models for readmissions in heart failure patients. By leveraging deep learning techniques, the researchers were able to improve the identification of patients with impending hospitalization and prompt early interventions. Equally inspiring research is taking place in Australia, where Monash University data analysts are applying AI prediction models to evaluate the risk of hospital readmissions for patients with chronic liver disease and heart failure.
Lack of in-house data analytics expertise
Many healthcare organizations struggle with extracting the full value of analytics-based PHM systems due to the shortage of relevant skills. To gain transparency into the entire continuum of community healthcare, PHM system users must understand how to prioritize and integrate droves of data sources and slice and dice the available information by dimensions they require.
Most healthcare personnel lack the capability and confidence to stratify populations, define patient cohorts, and report on outputs in a way consistent with their PHM needs. Without this knowledge, and without the understanding of how particular variables impact the outcomes delivered by data algorithms, they find handling healthcare analytics an insurmountable challenge.
Functional Capabilities of Optimized Population Health Management Systems
As the above specific challenges demonstrate, developing a comprehensive population healthcare management program presents many problems for medical organizations, especially those with scant resources and budget. The onus is on PHM vendors to address these issues by extending solutions with the following key capabilities:
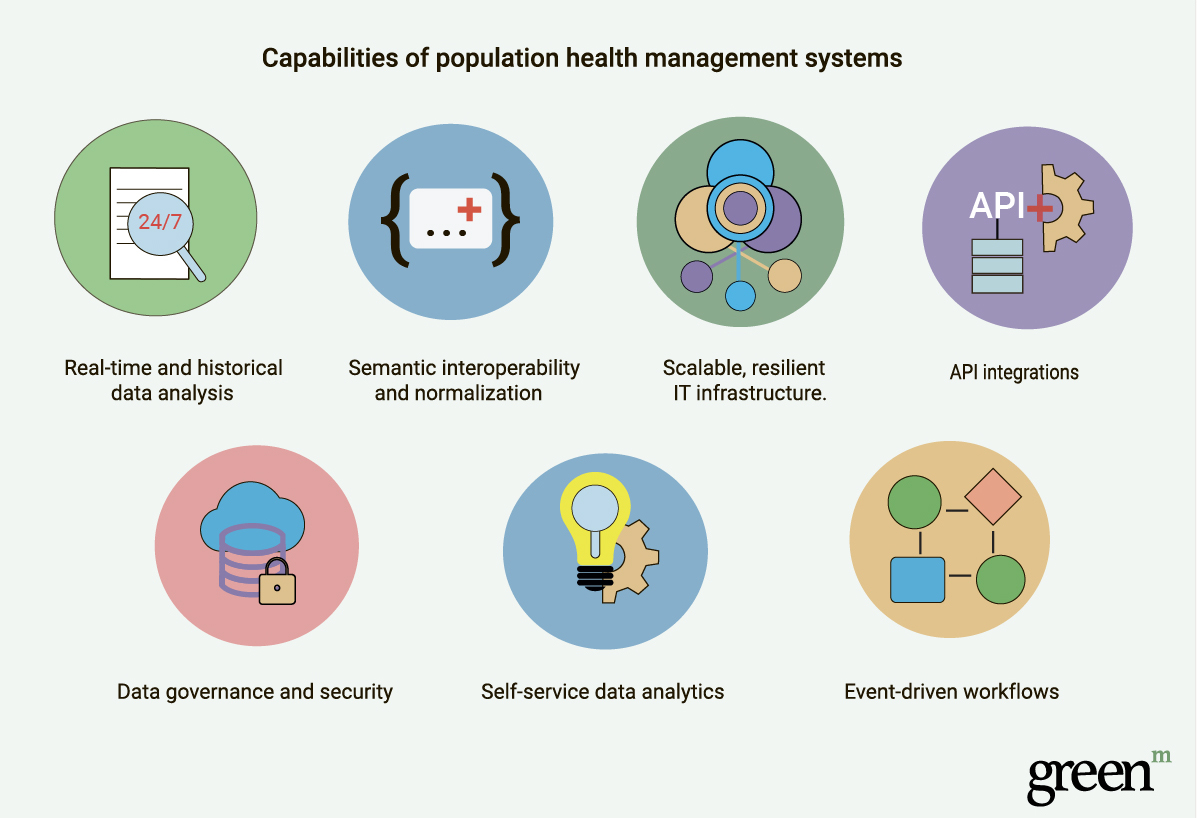
- Real-time and historical data analysis.
A fully-featured Population Health Management system generates actionable insights based on a combination of real-time and historical inputs. To adequately measure the impact of compounded determinants on public health outcomes and accurately assess hazard rates, it collects and updates information on the fly and performs an accurate analysis of historical data. Beyond simply collating integrated data from the past, a PHM platform should also provide the capability to align historical standard codes, understanding when a code is no longer valid, and knowing how to map it into a new one to keep data relevant.
- Semantic interoperability and normalization.
Population Health Management operates on disparate lexicons coming from a variety of data sources, each following different naming conventions. To avoid ambiguity and act as a single, integrated source of truth for providers, PHM systems need a powerful semantic translation engine, which recognizes and normalizes all captured data into standard terminologies. The essential features of such a tool include the cognition engine, semantic mapping, and customizable algorithms and workflows.
- Scalable, resilient IT infrastructure.
PHM systems must be able to grow as the needs of the targeted populations evolve. A reliable system should demonstrate the flexibility to combine information from various systems consistently and the ability to incorporate new data sets and new analytic modules. Whether a given solution can or cannot meet this requirement depends heavily on the solution architecture, which should be able to handle the ever-growing data volumes and complexity.
- API integrations.
Application Programming Interfaces provide a reliable, fast, and secure way to access third-party apps. They break down data silos, enabling providers to build new capabilities into their PHM system without too much engineering hassle. More importantly, through API integrations with Patient Portals and mHealth apps, PHM systems engage patients in a timely manner, involving them in decision-making and encouraging them to develop healthy habits. The support for API integrations is not so much of an add-on to compliant PHM systems, but rather a necessity mandated by the regulations; Meaningful Use Stage 3 states that a patient has the right to their electronic health information via API.
- Data governance and security.
Security is of foremost importance for all healthcare IT systems, including PHM solutions, as they store a host of highly sensitive patient data. Each medical facility and professional is obliged to follow fundamental data protection guidelines and regulations (such as using a VPN to access IT systems, applying secure password policies, or installing appropriate anti-malware software, etc.). Apart from these precautions, PHM solution vendors can step up security by embedding data governance into their system architecture and leveraging reliable cloud infrastructures that offer in-built security features.
- Self-service data analytics.
A well-designed PHM system should require as little effort as possible on the part of end-users, whether these are patients or medical staff. Solutions enhanced with a self-service analytics component empower users to input and analyze data unaided and generate insights without involving IT staff. They achieve this through crisp predefined dashboards that instantly address all the routine questions, as well as advanced built-in analytic capabilities enabling independent, on-demand deep research.
- Event-driven workflows.
Practical and evidence-based plans with automated workflows help medical providers increase the efficiency of care coordination. This is especially relevant in the case of complex clinical and financial tasks, involving numerous stakeholders and multiple factors affecting the health outcomes. An intelligent workflow system can radically simplify such tasks, guiding the entire healthcare team in developing plans that factor in all aspects of care.
Population Health Management: Solving the Data Conundrum
In 1914, physicians had to make life-and-death choices acting solely on a combination of their knowledge and gut feeling. And — as demonstrated by Dr. Jordan’s case — these means often proved insufficient to deliver efficient care.
Today, technology has become a powerful ally to medical professionals, providing innovative healthcare solutions that not only help them come up with the right diagnosis but also proactively monitor patients’ health. Data lies at the core of these innovations, so IT healthcare management solution vendors should strive to make it as accurate, secure, and easily accessible as possible. Otherwise, doctors will still be left to their own resources, just as they were over a hundred years ago.
References:
Health Affairs, Cooling The Hot Spots Where Child Hospitalization Rates Are High: A Neighborhood Approach To Population Health,
https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05496
PR Newswire, Population Health Management Market Size Worth $150.6 Billion by 2027: Grand View Research, Inc.,
NAHC, Value Transformation Framework
http://www.nachc.org/wp-content/uploads/2019/03/Risk-Stratification-Action-Guide-Mar-2019.pdf
CDC.gov, Health and Economic Costs of Chronic Diseases,
https://www.cdc.gov/chronicdisease/about/costs/index.htm
NCBI, A machine learning model to predict the risk of 30-day readmissions in patients with heart failure: a retrospective analysis of electronic medical records data
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6013959/
IBM, Data infrastructure for managing Population Health
https://www.ibm.com/downloads/cas/MOJDOKBW
Deloitte, The transition to integrated care. Population health management in England
https://www2.deloitte.com/uk/en/pages/public-sector/articles/population-health-management.html